Enhancing Your Vision
Guiding you toward the procedure that fits your unique needs, so you can see the world clearly and confidently.
As someone who has performed thousands of cataract surgeries on patients with Macular Degeneration (AMD), I understand the unique challenges and concerns that come with managing both conditions. You might be wondering if cataract surgery can still improve your vision despite having AMD, and that’s a question I’ve addressed countless times in my practice.
In this article, I’ll share my experience and insights on how cataracts and Macular Degeneration interact, what you can expect from cataract surgery if you have AMD, and some real-life examples from my patients to illustrate the potential outcomes. Together, we’ll explore whether cataract surgery is a viable option for you.

I’ve worked with patients at every stage of AMD, from early detection to advanced cases. The stage of your AMD will heavily influence what we can achieve with cataract surgery.
Every patient is different, and the specific stage of your AMD plays a key role in determining the potential benefits of cataract surgery.
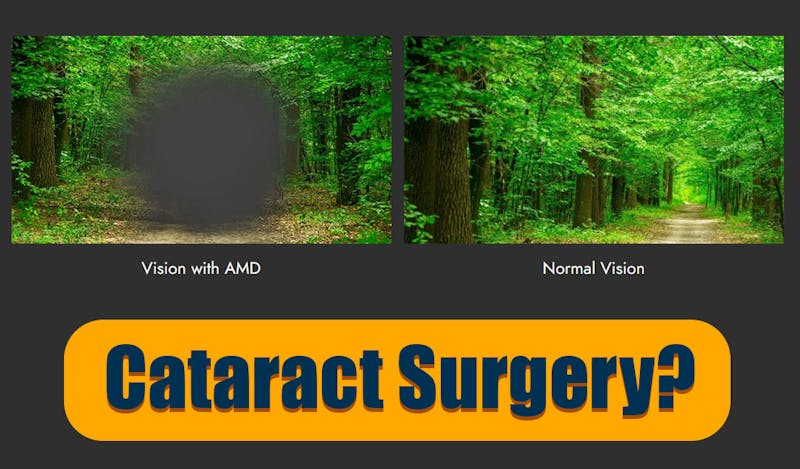
Cataract is clouding of the natural lens that physically blocks the light entry into the eye. Macular degeneration is a damage at the retinal level. Retina is the nerve tissue in the back of the eye that receives the light. They each effect your vision in a different way. However, their effect could be compounded to reduce your vision.
Having performed cataract surgery on many patients with AMD, I can tell you that the surgery can still offer significant benefits. By removing the cloudy lens, we can often improve your peripheral vision, reduce glare, and enhance overall visual clarity. This can make daily activities easier, even if your central vision is affected by AMD.
For patients with early to intermediate AMD, the improvements can be quite pronounced. However, if your AMD is more advanced, particularly in the late stage, the improvements may be more focused on quality-of-life enhancements rather than dramatic changes in central vision.
Another clear benefit of cataract surgery for patients with AMD is the fact that the retina specialist will have a better view of the back of the eye which is necessary for proper evaluation and treatment of their condition.
I’ve had patients like Mrs. Daftari, who had intermediate dry AMD and significant cataracts. After surgery, she experienced much better clarity and brightness in her vision, even though her central vision remained compromised. This improvement made a big difference in her ability to perform daily tasks.
In more advanced cases, like that of Mr. Wong with wet AMD, cataract surgery didn’t drastically improve his central vision, but it did reduce glare and improve peripheral vision, allowing him to navigate his environment more safely. These real-life examples show how cataract surgery can still provide meaningful enhancements to your vision, even with AMD.
Before we decide on cataract surgery, I always ensure a thorough assessment of your macula using Optical Coherence Tomography (OCT). This non-invasive imaging test gives us a detailed view of your retina, helping me to evaluate the extent of any macular damage and predict the likely benefits of surgery.
In my practice, OCT is invaluable for determining how much improvement in vision we can expect after cataract surgery. For instance, if your OCT shows that the macula is still relatively healthy, especially in the early or intermediate stages of AMD, we can often achieve significant improvements. If the OCT reveals more severe damage, particularly with fluid or bleeding in wet AMD, we adjust our expectations accordingly.
I also conduct a comprehensive retinal examination and often collaborate with a retina specialist to ensure the best possible outcome. This includes coordinating any ongoing AMD treatments, like anti-VEGF injections, with the timing of your cataract surgery. By working together, we can optimize your care and minimize the risk of complications.
Each step in this assessment process is crucial to setting realistic expectations and tailoring the surgical plan to your specific needs.
Given my extensive experience with AMD patients, I’ve developed a surgical approach that is especially gentle to protect your macula. I minimize the use of Phaco power during surgery, employ more gentle chopping techniques, and take extra care to avoid unnecessary contact with the iris or other parts of the eye that could increase inflammation. These techniques help reduce the risk of complications and ensure a smoother recovery for my patients with AMD, who have more sensitive maculas.
When it comes to choosing an intraocular lens (IOL), I make decisions based on the degree of your AMD. For those with less severe AMD who also like some degree of freedom from reading glasses, I might use an extended depth focus lens like the Vivity lens, which can provide better vision across different distances without compromising on clarity. However, for more advanced AMD, I typically recommend a monofocal lens to ensure the best possible outcome. I avoid multifocal lenses in these cases because they can sometimes reduce contrast sensitivity and increase glare, which could exacerbate AMD-related vision issues.
After surgery, I closely monitor all my patients, especially those with AMD. Regular follow-up visits allow me to track your recovery, manage any potential complications, and evaluate how well the surgery has improved your vision.
For patients with wet AMD, ongoing monitoring for any signs of disease activity is essential. If needed, we can continue treatments like anti-VEGF injections to help protect your vision. My goal is to provide comprehensive care that addresses both your cataracts and AMD, helping you achieve the best possible outcomes.
One of the most common misconceptions I encounter is the belief that cataract surgery will fully restore vision, even in the presence of AMD. While cataract surgery can significantly improve overall visual clarity, it cannot reverse the damage caused by AMD, particularly to central vision.
In my practice, I always make sure to set realistic expectations. For patients with AMD, the benefits of cataract surgery are often more about improving peripheral vision, reducing glare, and enhancing the quality of life, rather than completely restoring central vision. This is why it’s so important to have an open and honest discussion about what cataract surgery can achieve in your specific case.
Another misconception is that patients with AMD should avoid cataract surgery altogether. Some patients worry that the surgery might worsen their AMD or that the benefits won’t be worth it.
Based on my experience, I can tell you that even in cases of advanced AMD, cataract surgery can still provide meaningful improvements. For example, reducing the glare caused by cataracts can make a big difference in your ability to perform daily tasks and maintain your independence. While the improvements may not be as dramatic as they would be in someone without AMD, they can still significantly enhance your quality of life.
Mrs. Daftari came to me with intermediate dry AMD and cataracts in both eyes. She was struggling with daily tasks like reading and recognizing faces. After a thorough evaluation, including OCT imaging, we decided to proceed with cataract surgery using a monofocal lens to maximize her overall visual clarity.
Post-surgery, Mrs. Daftari noticed a significant improvement in her vision. While her central vision remained affected by AMD, the clarity and brightness of her overall vision improved, allowing her to better perform daily activities. This case highlights how cataract surgery can enhance the quality of life for patients with intermediate AMD.
Mr. Wong, who had advanced wet AMD, was experiencing significant vision loss and dense cataracts. We discussed the potential benefits and limitations of cataract surgery, and he understood that while his central vision might not improve significantly, the surgery could still help with peripheral vision and reduce glare.
We proceeded with the surgery, using a monofocal lens, and the results were as expected. Mr. Wong reported that his ability to see in his peripheral vision improved, and glare was significantly reduced, making it easier for him to navigate his environment. Although his central vision remained compromised, the overall improvement in his vision made a difference in his daily life.
These case studies show how cataract surgery, even in patients with Macular Degeneration, can offer valuable benefits. Each case is unique, and by tailoring the surgical approach to the specific needs of the patient, we can often achieve outcomes that significantly enhance daily functioning and overall quality of life.
Guiding you toward the procedure that fits your unique needs, so you can see the world clearly and confidently.




If you do not see your preferred date and time please call the office, so we can accommodate your request (917) 398-4011.